
What to expect:
Lifestyle modifications, such as sustainable weight loss, are interventions general practitioners can encourage in their patients to mitigate risk of cardiovascular disease (CVD).1,2 But initiating a cardiovascular health assessment and opening the discussion on risk factors can be tricky. How can we communicate and offer support to patients in a way that motivates adherence to a healthier lifestyle, reducing the risk of CVD?
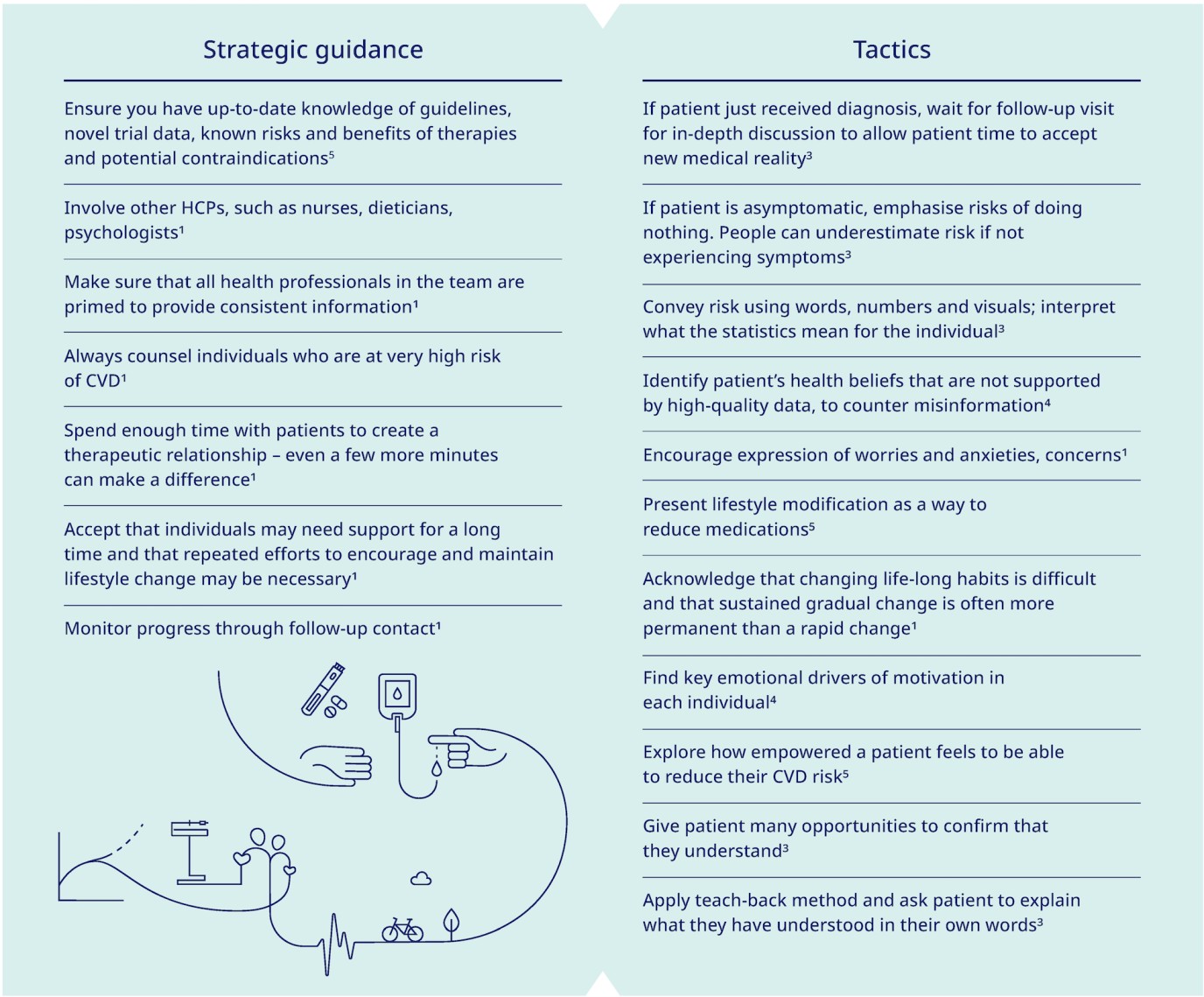
Current guidelines on cardiovascular disease emphasise the value of engaging patients in discussion about CVD risk factors.1,5
But talking about risk in a cardiovascular health assessment is not simply about delivering information.3 Risk conversations need to be informed by a patient’s health literacy, level of trust, emotions and readiness to know more.3
Cardiovascular assessments and education on risk should be handled proactively but in a sensitive manner. Clinicians should help their patients understand cardiovascular risk scores and recognize what it means to them as individuals.
From patient education to patient motivation
While cardiovascular assessments and education on risk have been the traditional focus of prevention and protection from cardiovascular disease, patient adherence to interventions, such as lifestyle changes and medication, remains a key challenge.4
A recent review on improving patient adherence in CVD prevention proposes a novel approach - shifting away from educating patients, to identifying key individual motivators.4 As the public has caught up with understanding the need to stop smoking, start exercising and eating less processed food, patients require a shift in focus - from what they know rationally, to what matters to them on an individual level.4 Motivational techniques in the treatment of substance abuse disorders using a “collaborative conversational style” are becoming more popular to strengthen the patient’s own motivation and commitment to change.4
Principles of motivational interviewing6
- Open questions – to explore what individual already knows; clinician offers what they know
- Affirmation – clinician is non-judgmental, affirms individual’s inner resources to build confidence in ability to change
- Reflection - clinician listens, interprets what individual is expressing
- Summarising – by clinician ensures shared understanding, reinforces key points
What can you do to further motivate your patients?4
To read more, including tips and resources visit:
Training:
To expand your professional learning about obesity and cardiovascular disease (CVD), register for SCOPE e-learning for CME-accredited training modules.
Toolkits:
American College of Cardiology Communication toolkit: Improving Cardiovascular Risk Communications. Available at: https://www.acc.org/~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/Tools%20and%20Practice%20Support/Risk-Communications/2%20Full%20Toolkit.pdf?la=en. Last accessed: September 2022.
Centers for Disease Control and Prevention Heart Disease Communication Toolkit: Available at: https://www.cdc.gov/heartdisease/communications_kit.htm. Last accessed: September 2022.
Guidelines:
European guidelines on cardiovascular disease prevention in clinical practice (2016). Available at: https://academic.oup.com/eurheartj/article/37/29/2315/1748952. Last accessed: September 2022.
American Heart Association guidelines (2021). Available at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000973. Last accessed: September 2022.
World Health Organization. Global atlas on cardiovascular disease prevention and control (2011). Available at: https://apps.who.int/iris/handle/10665/44701. Last accessed: September 2022.
HQ22OB00148, Approval date October 2022
The site you are entering is not the property of, nor managed by, Novo Nordisk. Novo Nordisk assumes no responsibility for the content of sites not managed by Novo Nordisk. Furthermore, Novo Nordisk is not responsible for, nor does it have control over, the privacy policies of these sites.
At Novo Nordisk we want to provide Healthcare Professionals (HCPs) with scientific information, resources and tools.
