
What to expect:
Even a modest weight loss can have positive effects, reducing risk factors and ultimately preventing a cardiovascular disease diagnosis.1,2,3 The link between weight loss and improvements in cardiovascular risk factors has been demonstrated in both observational studies and randomised control trials.3-9 Research has shown that weight loss lowers hypertension, insulin resistance, dyslipidaemia and inflammation and improves levels of triglycerides, cholesterol, and blood glucose in people with overweight and obesity.3,8–11 Moreover, people with type 2 diabetes and obesity show significant improvement in their condition with weight loss, reverting to non-diabetic blood glucose levels and achieving remission.9
What to expect:
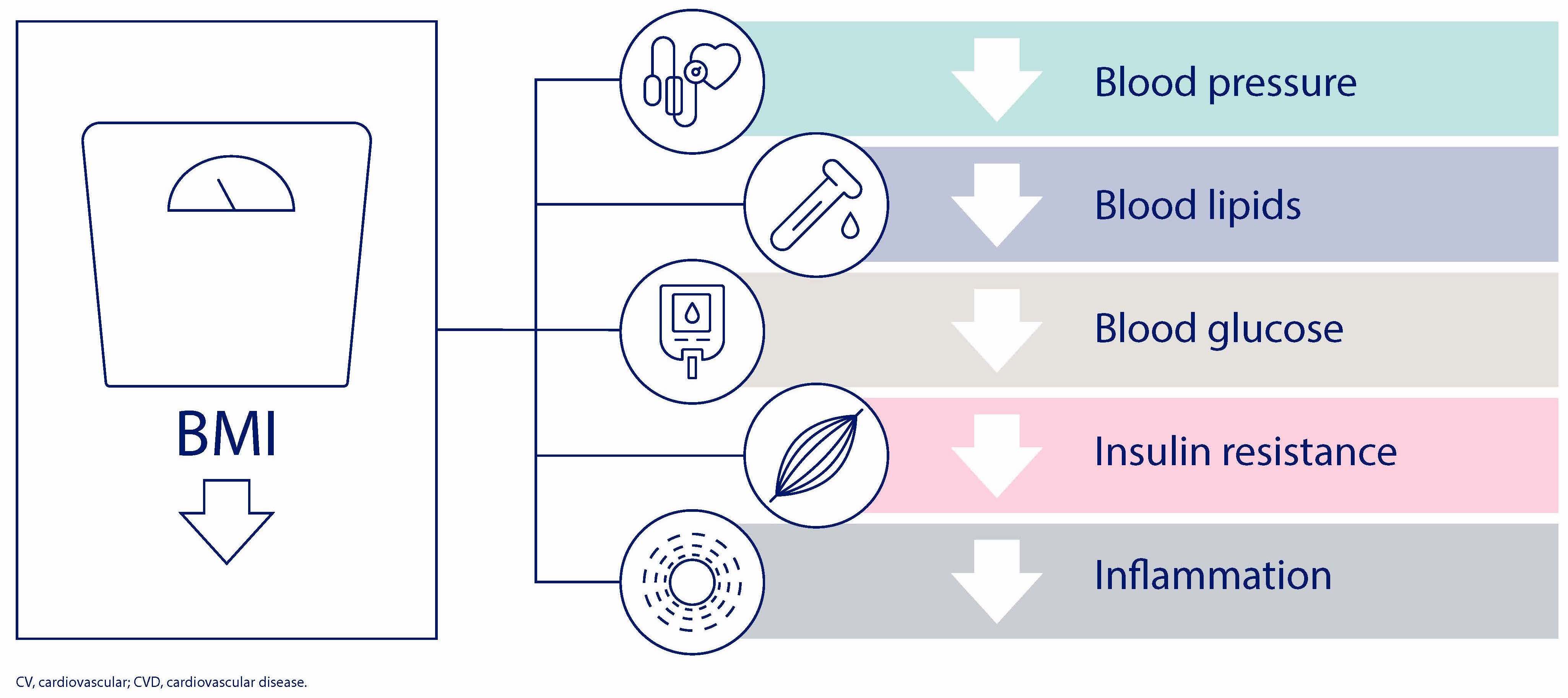
Weight loss and reducing body mass index (BMI) improve CVD risk factors, lowering blood pressure, blood lipids, blood glucose, insulin resistance and inflammation.2,11
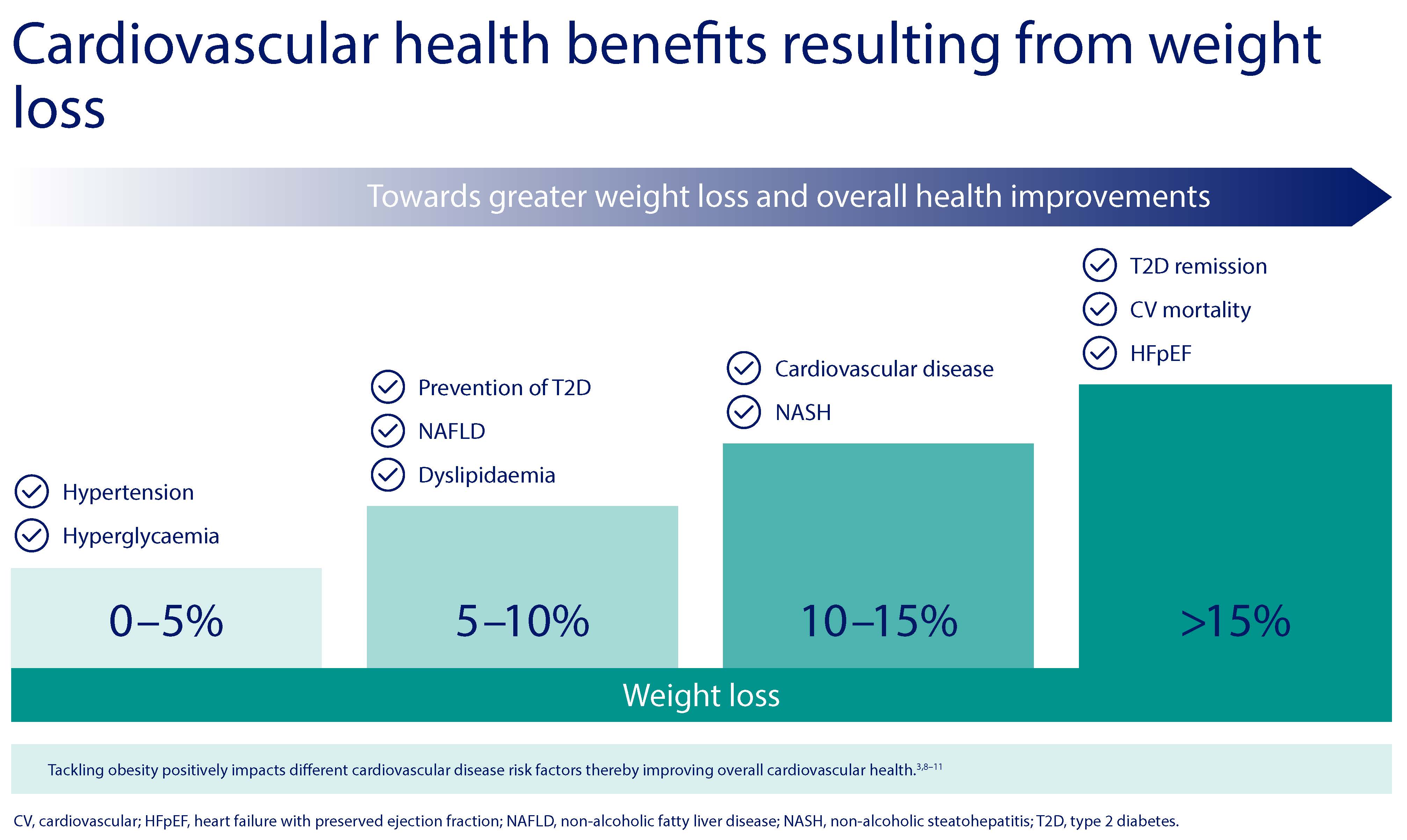
The degree of benefit in terms of reduction of CVD risk factors and poor outcomes increases with higher percentage of weight loss.3,4,7,8
Modest weight loss of 5% is associated with reduction in systolic and diastolic blood pressure and reduced hyperglycaemia/HbA1c.3 Even a weight loss of only 4.5kg in people who were between 110% and 165% of their ideal weight at baseline with stage 1 hypertension of less than 140 mm Hg systolic and 83–89 mm Hg diastolic can achieve clinically significant long-term reductions in blood pressure with reduced risk for hypertension.4 Each 1 kg weight loss is associated with 0.2 mmol/mol reduction in HbA1c, or 0.6 mmol/mol in people with diabetes.5 Improvement in glycaemia from weight loss has also been noted in the early stage of diabetes, when individuals still have a relatively preserved insulin secretion capacity.6
5-10% weight loss is associated with a reduction of intrahepatocellular lipids in non-alcoholic fatty liver disease; reduction in triglycerides, increase in HDL cholesterol, reduction in non-HDL cholesterol and prevention of type 2 diabetes.3,7
10-15% weight loss results in improvements in major cardiovascular disease events, even in patients already diagnosed with type 2 diabetes.3,8 In a sub-analysis of individuals in the Look Ahead trial who had overweight or obesity and type 2 diabetes and lost 10% or more of their body weight, there was a 21% decrease in CVD death, non-fatal acute myocardial infarction, non-fatal stroke, or hospitalisation for angina, compared with those who lost less than 10%.8 The same group had a 24% reduction when the outcome was expanded to include coronary artery bypass grafting, carotid endarterectomy, percutaneous coronary intervention, admission to hospital for congestive heart failure, peripheral vascular disease, and total mortality.
Greater than 15% weight loss can lead to remission of type 2 diabetes, especially when diabetes duration is short, improvements in heart failure with preserved ejection fraction and reductions in cardiovascular mortality.9,10,11
The 2020 Canadian Adult Obesity Clinical Practice Guidelines describe obesity management and cardiorespiratory fitness as “critically important” in improving the overall cardiovascular health of people who have overweight and obesity.12 The guidelines confirm that obesity management benefits all patients with obesity, regardless of the amount of weight loss.12
For more information on interventions to address cardiovascular risk in patients with obesity, click here.
HQ22OB00146, Approval date: October 2022
The site you are entering is not the property of, nor managed by, Novo Nordisk. Novo Nordisk assumes no responsibility for the content of sites not managed by Novo Nordisk. Furthermore, Novo Nordisk is not responsible for, nor does it have control over, the privacy policies of these sites.
At Novo Nordisk we want to provide Healthcare Professionals (HCPs) with scientific information, resources and tools.
