What to expect:

What to expect:
Obesity is much more than just excess weight. It is associated with over 200 complications affecting an individual’s health and various organ systems.1-8
Consequently, obesity has a significant association with morbidity and mortality. Severe obesity has been associated with a decreased life expectancy and increased rate of death independently of age, geographic region, educational qualification or smoking.9 This includes greater risk of developing diabetes,10 hypertension10 and hyperlipidaemia11. Heart failure12, metabolic syndrome13 and ischemic stroke14 are other significant and well-evidenced complications of obesity. Obesity also increases mortality from a number of cancers, including for example breast cancer10 and prostate cancer10. Similarly, individuals with obesity are at greater risk to experience depression,15 other mental health problems15 and overall decreased quality of life.15
The high rate of obesity-related comorbidities emphasises how important early intervention is in order to prevent serious outcomes.
Click on any of the complications below for more information on their association with obesity and the impact of health.
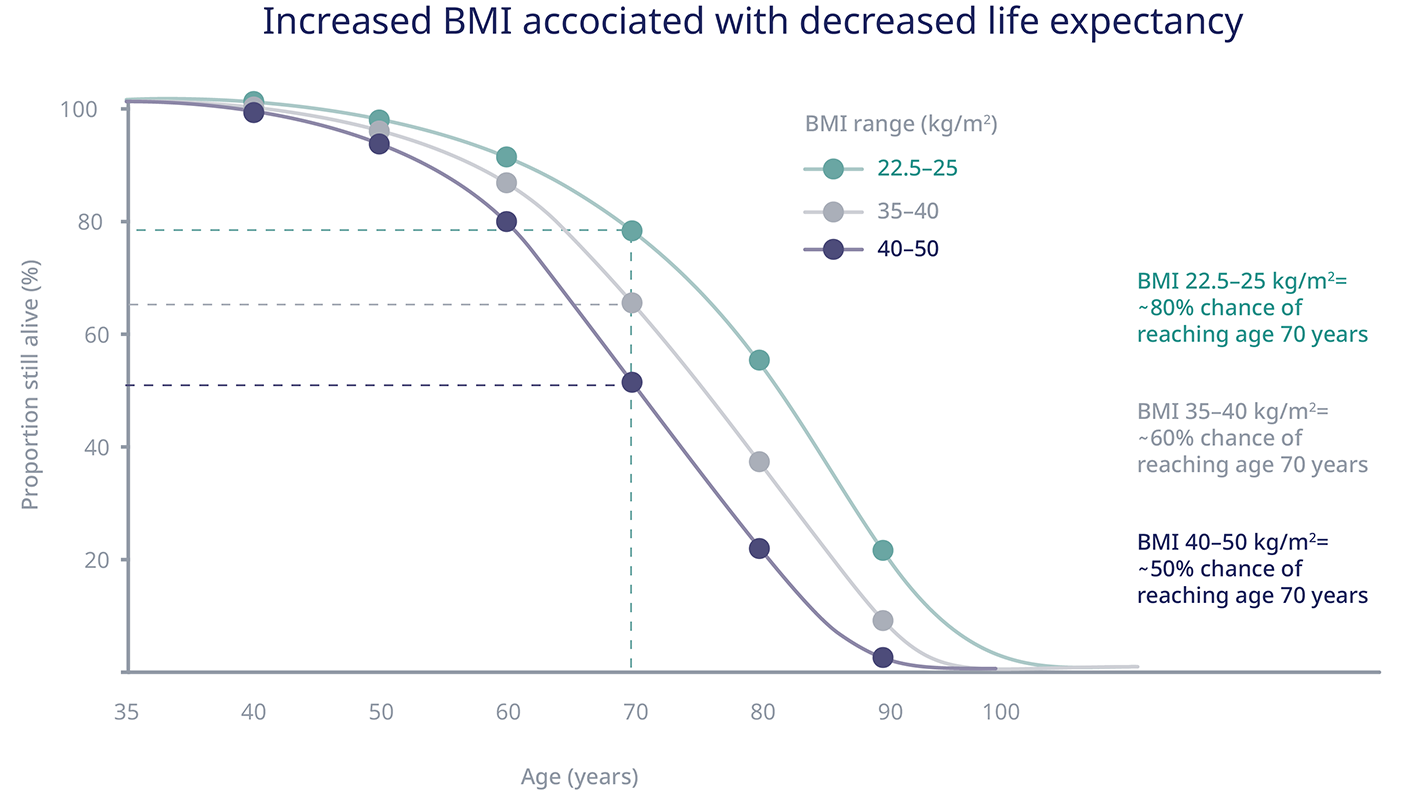
The adverse consequences of obesity, obesity-related diseases and issues around obesity, across all areas of health, mean that the condition also decreases lifespans.46
Research shows that a high BMI is associated with a decreased life expectancy of up to 10 years.47 For every 5 kg/m2 BMI increment above the range of 22.5–25.0 kg/m2, there is a 30% increase in overall mortality.47
Conditions caused by obesity and their determinants are complex, leading to numerous comorbidities and medical complications. But advances in healthcare have provided us with a range of tools and ways to better treat obesity.
You can download practical step-by-step guides for the treatment of obesity both in adults and children by clicking the Download button below.
If you found these resources valuable, click on the envelope icon above to share them with your colleagues, and support other medical professionals in their daily practice.
Interested to discover more useful resources? Discover our
comprehensive collection of obesity
resources now.
HQ22OB00119, Approval date: June 2022
The site you are entering is not the property of, nor managed by, Novo Nordisk. Novo Nordisk assumes no responsibility for the content of sites not managed by Novo Nordisk. Furthermore, Novo Nordisk is not responsible for, nor does it have control over, the privacy policies of these sites.
At Novo Nordisk we want to provide Healthcare Professionals (HCPs) with scientific information, resources and tools.